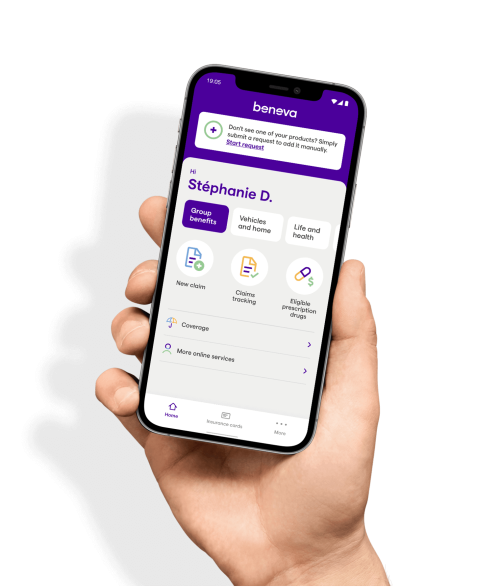
Not sure if your prescription drug is covered under your insurance plan?
Use our simulation tool in the Client Centre to find out if a prescription drug you’ve been prescribed is covered by your group insurance plan, and if it requires prior authorization.
